Diabetes. It’s a term you’ve likely heard before, and it’s a condition that affects a whopping 10.5 percent of the American population, according to the American Diabetes Association. What’s more intriguing is how the role of insulin, a hormone that you may know less about, plays a huge part in managing this chronic illness. In this article, you’ll delve deep into the multifaceted relationship between insulin and diabetes.
The Basics: Understanding Diabetes and Insulin
For starters, let’s lay out some basic facts. You might already know that diabetes is a chronic illness characterized by high levels of glucose in the blood. This condition is categorized mainly into two types, Type 1 and Type 2 diabetes.
In Type 1 diabetes, the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas, resulting in little to no insulin production. On the other hand, the more common Type 2 diabetes is characterized by insulin resistance, where the body still produces insulin but is unable to use it effectively.
In both cases, the result is the same: too much glucose in your bloodstream and not enough in your cells, where it serves as a vital source of energy.
But what about insulin? What role does it play?
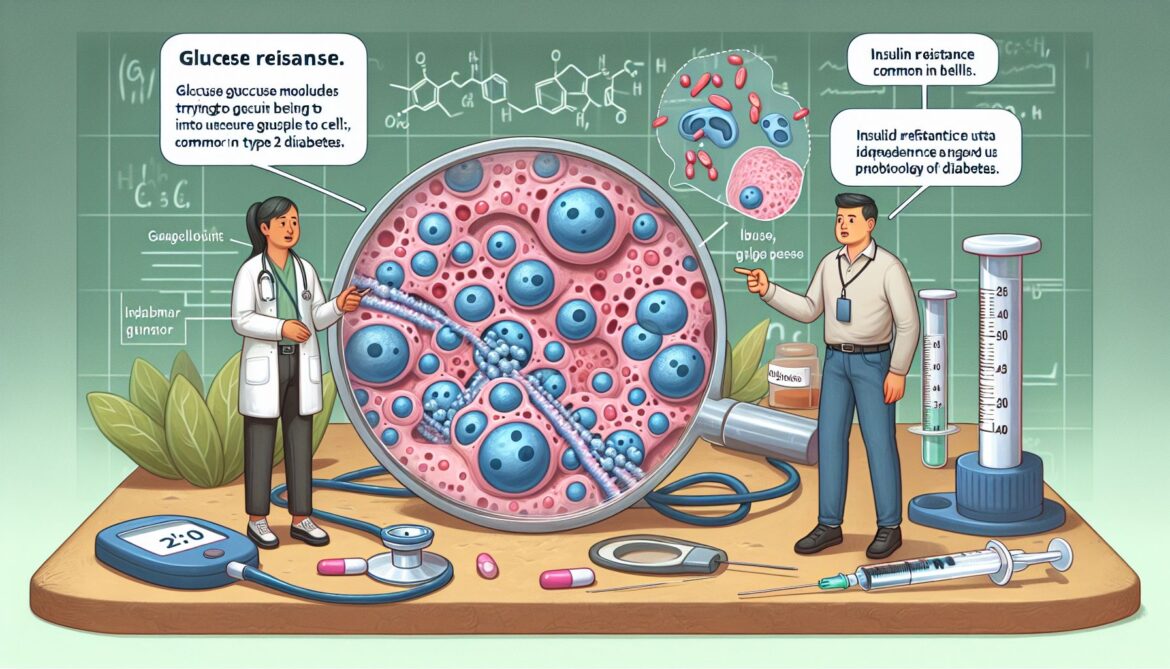
Insulin, simply put, is a hormone. It’s a chemical messenger responsible for ensuring that glucose gets to where it needs to go. After you eat, your blood sugar levels rise, triggering the production of insulin. This hormone then acts as a key, unlocking your body’s cells to let the glucose in. Without a sufficient amount of insulin, glucose can’t enter the cells and remains circulating in the bloodstream, causing elevated blood sugar levels.
The Importance of Insulin Management in Diabetes
Now that you understand the role of insulin, it’s time to look at how it’s controlled in people living with diabetes.
When the body can’t produce enough insulin or use it effectively, it’s necessary to provide it externally, which is done in the form of insulin injections or an insulin pump. For individuals with Type 1 diabetes, insulin therapy is a lifelong necessity. Those with Type 2 diabetes might also need insulin therapy if other treatments fail to keep blood glucose levels in check.
Just injecting insulin doesn’t solve the problem, though. You’ll need to continuously manage your blood glucose levels to ensure they don’t go too high or too low. You can do this through regular monitoring, adjusting your insulin doses according to the amount of carbohydrates consumed or physical activity performed.
Challenges in Insulin Therapy and Management
Undeniably, there are challenges associated with insulin therapy. The regular monitoring of blood glucose levels, counting carbs, the fear of low blood sugar, and the inconvenience of always having to carry around insulin and supplies are just a few of these challenges.
Additionally, insulin therapy costs can be prohibitive for many. A study published in the Journal of the American Medical Association found the cost of insulin nearly doubled between 2012 and 2016, leading to increased financial burdens for those affected.
Yet another challenge in insulin therapy lies in achieving good glycemic control without hypoglycemia (low blood sugar). An overdose of insulin can lead to hypoglycemia, a dangerous condition that can cause seizures, unconsciousness, and and in severe cases, death.
The Future of Insulin Therapy
Despite these challenges, advancements in technology continue to shape the way we understand and treat diabetes. Insulin pumps and continuous glucose monitoring systems that provide real-time blood glucose levels are improving the lives of those with diabetes. New types of insulin are being developed as well, with faster onset and longer durations.
One promising development is in the field of glucose-responsive insulin, sometimes called ‘smart insulin.’ This next-generation insulin would respond to increasing blood glucose levels and automatically adjust its activity, reducing the burden of management and reliance on external monitoring. While human trials have yet to begin, the future of insulin therapy is looking encouraging.
Wrapping up: The Takeaway on Insulin and Diabetes
Understanding the complex relationship between insulin and diabetes is not just about knowing a disease – it’s about understanding a condition that affects millions of lives every day. Proper management of insulin is key to leading a healthy life with diabetes, but it’s also not without its own set of challenges.
However, innovations and advancements in the field hold promise for the future. As we continue to delve into the relationship between diabetes and insulin, a better, more manageable life for those living with diabetes becomes a more achievable reality. And that’s something to look forward to.