If someone would mention the most crucial elements in managing diabetes, insulin would undoubtedly top the list. It’s not just an essential hormone produced by the human body, but it also plays a prominent role in regulating blood glucose levels. Globally, we find that an estimated 422 million people are fighting diabetes, making it a significant worldwide health concern [^1^]. Understanding the connection between insulin and diabetes could shed more light on how to manage this chronic condition.
Insulin: A Brief Overview
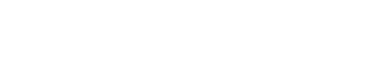
Knowing more about insulin and its functions is a crucial step towards understanding the relationship between insulin and diabetes. Produced in your pancreas, specifically the beta cells in the islets of Langerhans, insulin takes responsibility for letting your body cells absorb glucose from your bloodstream. This crucial process provides the necessary energy your body needs for everyday operations.
However, the stakes would rise if your body fails to produce the needed insulin or could not utilize it, leading to serious health consequences like diabetes.
Understanding Diabetes
When your body isn’t making enough insulin or fails to utilize it efficiently, you’re headed towards diabetes. It puts you at risk by increasing your blood glucose levels, which then plays havoc with many bodily functions and organs such as your heart, kidneys, or eyes.
There are two primary types of diabetes you need to be aware of:
Type 1 Diabetes
Understanding type 1 diabetes begins with realizing it as an autoimmune disorder where your body’s immune system wreaks havoc on your insulin-producing pancreatic cells. With little to no insulin, glucose accumulates in your blood instead of supplying energy to the cells. Worldwide, you’ll find that approximately 10% of all people with diabetes are diagnosed with type 1 [^2^].
Type 2 Diabetes
Accounting for the majority of all diabetes cases, type 2 diabetes appears when your body resists the effects of insulin or doesn’t produce enough insulin to maintain normal blood glucose levels.
Diabetes Management: The Role of Insulin
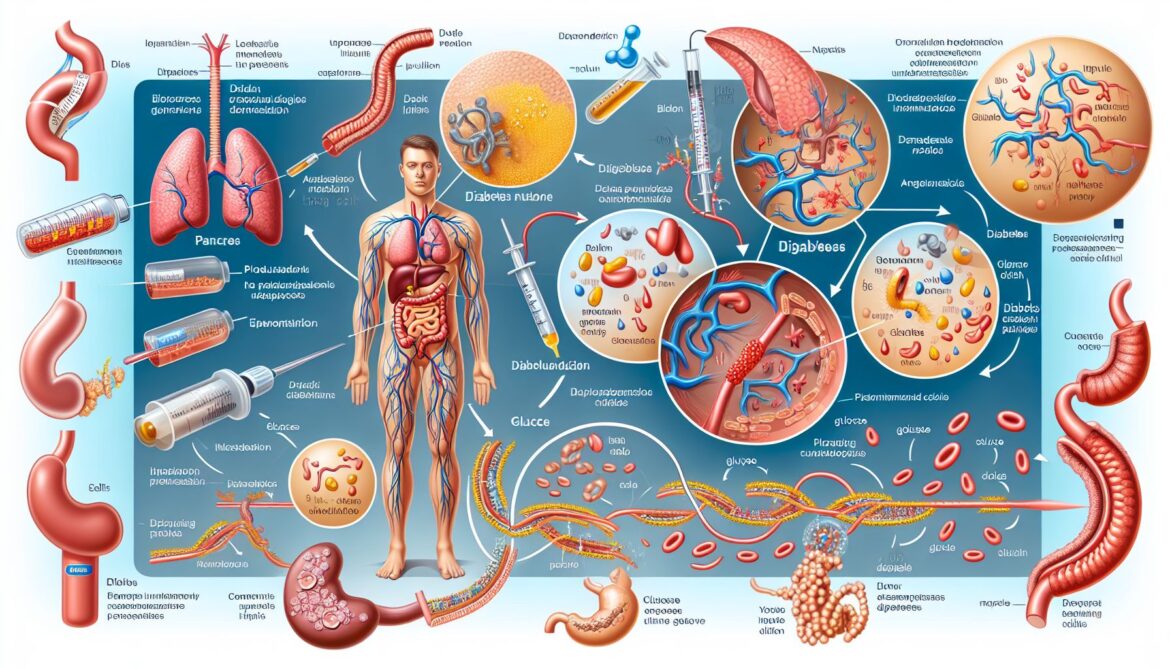
Regardless of the diabetes type, dealing with this chronic condition always entails insulin regulation. This point is especially applicable for type 1 diabetes, where patients must take exogenous insulin to compensate for the insulin their bodies cannot produce.
The main goal of exogenous insulin therapy is to imitate the body’s natural insulin patterns as closely as possible. This therapy should be tailored to your personal needs, and it often includes various insulin types: long-acting (basal) insulin, and fast-acting (bolus) insulin.
Insulin Therapy for Type 1 Diabetes
For people with type 1 diabetes, insulin injections are part and parcel of everyday life. Given the body’s inability to produce the hormone, the only way to maintain healthy glucose levels is to provide the body with outside insulin.
There are various ways of administering insulin, such as through injections, insulin pens, or insulin pumps. While injections usually require multiple pricks each day, the insulin pump keeps releasing insulin in your body continuously.
Insulin and Type 2 Diabetes
Even if type 2 diabetes patients don’t need insulin at the onset of their condition, over time, they might need to incorporate insulin therapy into their treatment. This need arises as the disease progresses and your body gradually loses its ability to produce insulin.
Insulin therapy can go hand in hand with other diabetes medications and lifestyle changes like diet adjustments and regular exercise.
Put Insulin in Your Diabetes Management Plan
Dealing with diabetes doesn’t just entail monitoring meals or being physically active—it also includes developing an understanding of insulin’s role. Beyond knowing about symptoms or complications, it’s about acknowledging the complex relationship between insulin and diabetes.
By understanding how insulin functions in your body and how it affects your blood glucose levels, you’re better equipped to manage your diabetes. It gives you not just firm control over your current health status but also arms you with the knowledge to prevent potential complications in the future.
By staying proactive in learning about the relationship between insulin and diabetes, harnessing this knowledge, and maintaining an open dialogue with your healthcare team, you’re paving a smoother path in your journey with diabetes.
[^1^]: World Health Organization (2021). Diabetes. [^2^]: Diabetes.co.uk (2020). Type 1 Diabetes.