You might have heard of insulin and diabetes, but may not fully understand how they are related. Diabetes is a chronic disease that affects the way your body regulates blood sugar, or glucose. When it comes to managing this disease, insulin plays a fundamental role. Let’s dive into the complex relationship between insulin and diabetes.
Understanding Insulin: The Key to Unlocking Sugar
Insulin is a hormone produced by the pancreas. It acts as a key for glucose to enter your cells. When you consume food, your body breaks it down into glucose and other nutrients. This glucose enters your bloodstream and raises your blood sugar levels. In response, your pancreas produces insulin. This hormone allows glucose to be absorbed by your cells, where it’s used for energy.
Without insulin, the glucose remains in your bloodstream, leading to high blood sugar levels. Over time, these elevated blood sugar levels can cause serious health complications such as heart disease, stroke, kidney disease, eye disease, nerve damage, and even amputation of limbs.
The Critical Role of Insulin in Diabetes
When it comes to insulin’s role in diabetes, there’s a crucial distinction between Type 1 and Type 2 diabetes.
Type 1 Diabetes and Insulin
In Type 1 diabetes, the body’s immune system mistakenly destroys the insulin-producing cells in the pancreas. According to the American Diabetes Association[Link to the American Diabetes Association], around 1.6 million Americans are living currently with this form of diabetes, including about 187,000 children and adolescents.
Without insulin, glucose cannot enter the cells, leading to an accumulation of glucose in the bloodstream while the body’s cells literally starve for energy.
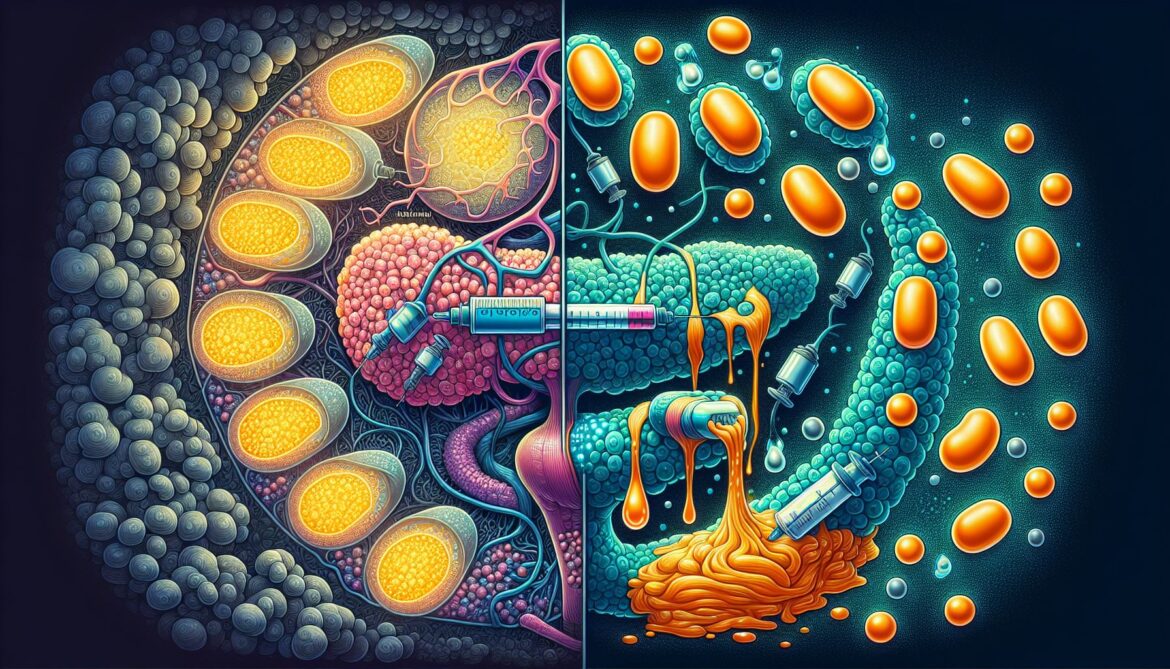
Individuals with Type 1 diabetes require lifelong insulin treatment. This usually involves multiple daily injections or the use of an insulin pump. Regular blood sugar monitoring is crucial for these patients to adjust their insulin doses.
Type 2 Diabetes and Insulin
In contrast, individuals with Type 2 diabetes do produce insulin, but their body’s cells become resistant to its effects. As a result, the pancreas produces more insulin to compensate. Over time, the pancreas can’t keep up with demand, and blood sugar levels rise.
According to the Centers for Disease Control and Prevention, 90 to 95 percent of the 34.2 million Americans with diabetes have Type 2. It’s more common in adults, but increasingly affecting children as well.
Insulin resistance can sometimes be managed with lifestyle changes such as regular exercise, a balanced diet, and weight loss. However, many people with Type 2 diabetes will eventually need medication such as metformin, insulin, or others to keep their blood sugar levels under control.
Innovations in Insulin Therapy
Over the years, insulin therapy has seen significant advancements, improving the lives of many people with diabetes. It’s crucial to remember that insulin isn’t a cure for diabetes, but a vital tool for management.
In the early days, insulin injections were painful and inconvenient, but the advent of insulin pens and pumps has made administering insulin much easier. These devices are portable, discreet, and typically less painful than traditional syringes.
Another innovative development is the variety of insulin types now available, including:
- Rapid-acting insulin, which starts to work within 15 minutes of injection and is typically taken before a meal.
- Long-acting insulin, which works for 24 hours or longer and is often used in combination with rapid-acting insulin.
There’s also been progress in the development of “artificial pancreas” systems. These systems constantly monitor your blood sugar levels and automatically adjust insulin delivery. This technology promises to revolutionize diabetes management in the future.
The Takeaway
The relationship between insulin and diabetes is complex and multifaceted. It’s important to understand this relationship to take control of your diabetes management or support loved ones living with the disease. Through continued research and technological advancements, managing diabetes and insulin therapy is becoming easier and more efficient. Always remember, effective management of diabetes requires a comprehensive approach, including proper medication, diet, exercise, and regular monitoring of blood glucose levels.
Sources:
The American Diabetes Association
Centers for Disease Control and Prevention